Hemophilia is a disorder of the blood that makes it hard for the body to stop bleeding because a good blood clot can’t be made. When bleeding occurs, the body has many proteins and cells that come to fix the problem by making a blood clot where the bleeding. The proteins that help stop bleeding are called clotting proteins. If the body does not have enough of one of the clotting proteins (also called factor proteins), it is hard for the body to stop bleeding. When someone has Hemophilia A, do not have enough, of the clotting protein called Factor VIII (8). When someone has Hemophilia B, they do not have enough, of the clotting protein called Factor IX (9). Hemophilia only affects the making of a clot, not how fast the body bleeds. Bleeding may last longer or may restart minutes, hours or days after stopping.
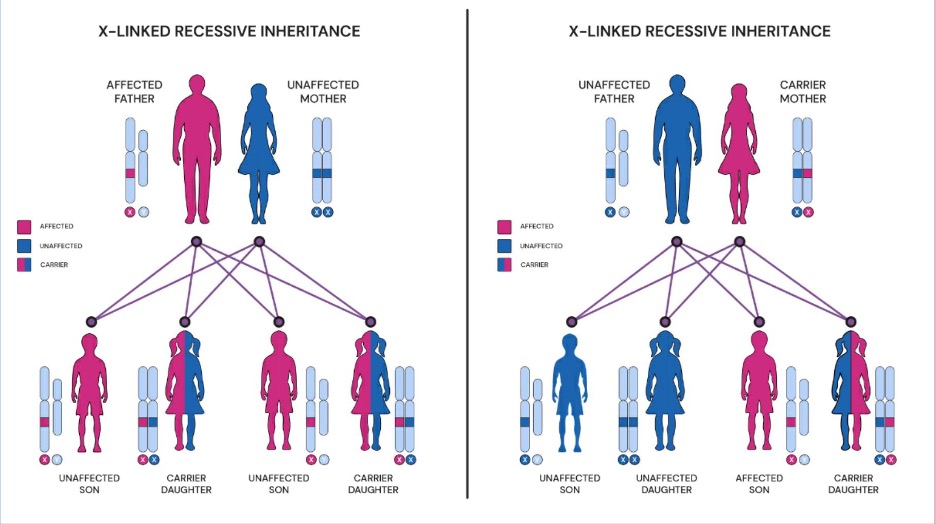
Hemophilia occurs mostly in someone born male. One of every 5,000 males born in the United States has hemophilia. Someone that is born female are carriers of the hemophilia gene and usually do not get hemophilia because usually only one of their chromosomes has the hemophilia gene. The chromosome that does not have the hemophilia gene will instruct the body to make clotting factors. It used to be thought that carriers of hemophilia do not have bleeding problems. That is not true! Carriers can have bleeding problems depending on their clotting factor levels. Sometimes the amount of clotting factor that is made by the one normal chromosome is not enough, and bleeding problems occur in carriers.